Key Takeaways
- OCD intrusive thoughts feel urgent and distressing, but specific cognitive techniques can interrupt the cycle and reduce their intensity in the moment.
- Grounding exercises like the 5-4-3-2-1 method and controlled breathing help shift focus away from obsessive thoughts by anchoring you in the present moment.
- Exposure and Response Prevention (ERP) therapy trains your brain to tolerate intrusive thoughts without performing compulsions, reducing their power over time.
- Thought labeling and cognitive defusion techniques from CBT help create distance between you and your OCD thoughts, making them easier to manage.
- A Mission For Michael provides specialized OCD treatment using evidence-based therapies like CBT, ERP, and EMDR in comfortable residential and outpatient settings.
Understanding OCD Intrusive Thoughts
Obsessive-compulsive disorder involves persistent, unwanted thoughts that create significant anxiety. These intrusive thoughts feel real and urgent, triggering compulsive behaviors as attempts to neutralize the distress. The challenge is that the brain misinterprets these thoughts as threats requiring immediate action. However, targeted cognitive strategies can interrupt this cycle immediately.
Recognizing that OCD thoughts are symptoms of a treatable condition—not reflections of reality or character—is the first step toward managing them. While medication can help some individuals, evidence-based psychological treatments provide powerful tools for interrupting the OCD cycle without pharmaceutical intervention.
Founded in 2010, A Mission For Michael (AMFM) offers specialized mental health care across California, Minnesota, and Virginia. Our accredited facilities provide residential and outpatient programs, utilizing evidence-based therapies such as CBT, DBT, and EMDR.
Our dedicated team of licensed professionals ensures every client receives the best care possible, supported by accreditation from The Joint Commission. We are committed to safety and personalized treatment plans.
Immediate Techniques to Stop OCD Thoughts
The 5-4-3-2-1 Grounding Method
This sensory awareness exercise interrupts obsessive thought patterns by redirecting attention to your physical environment. Identify five things you can see, four things you can touch, three things you can hear, two things you can smell, and one thing you can taste. The technique works by engaging your prefrontal cortex in present-moment observation, which competes with the brain regions generating intrusive thoughts. Practice this exercise as soon as you notice an OCD thought beginning to spiral.
Controlled Breathing Exercises
Anxiety amplifies OCD thoughts, creating a cycle that further increases distress. Breaking this cycle requires physiological intervention. Box breathing involves inhaling for four counts, holding for four, exhaling for four, and holding again for four. This pattern activates your parasympathetic nervous system, which counteracts the fight-or-flight response that OCD thoughts trigger. Regular practice strengthens your ability to deploy this technique during high-anxiety moments.
Thought Labeling
Rather than engaging with intrusive thoughts as if they’re factual, label them as OCD symptoms. Simply noting “that’s an OCD thought” creates cognitive distance. This strategy comes from mindfulness-based cognitive therapy and helps prevent the fusion between you and your thoughts. The label reminds you that these thoughts represent brain glitches rather than accurate information requiring action or analysis.
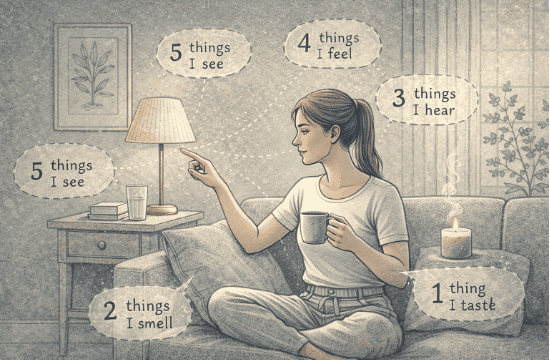
Grounding techniques like the 5-4-3-2-1 method and controlled breathing exercises provide immediate relief by redirecting your brain’s attention away from intrusive thoughts to present-moment sensory experiences.
Cognitive Techniques for Managing OCD
Cognitive Defusion
OCD gains power through thought-action fusion—the belief that thinking something makes it likely or meaningful. Cognitive defusion techniques deliberately make thoughts seem less important. Try repeating an intrusive thought rapidly for 30 seconds until it loses meaning, or imagine the thought written in a silly font or sung to a funny tune. These exercises train your brain to recognize thoughts as mental events rather than commands.
The Postponement Strategy
Tell yourself you’ll give the OCD thought attention in 15 minutes. Often, the urgency fades before the time arrives. This technique works because OCD thrives on immediate compulsion. Delaying engagement demonstrates that the feared outcome doesn’t occur just because you didn’t respond instantly. Over time, postponement intervals can extend, and many thoughts lose their grip entirely.
Response Prevention
The compulsion, whether mental or physical, provides temporary relief but strengthens the OCD cycle. Response prevention involves noticing the urge to perform a compulsion and choosing not to act on it. Start with minor compulsions and gradually progress to more challenging ones. The anxiety will initially increase but typically peaks within 20 to 60 minutes before naturally declining. This process, called habituation, teaches your brain that the feared consequence doesn’t materialize without the compulsion.
Response prevention and thought postponement strategies break the OCD cycle by teaching your brain that intrusive thoughts don’t require immediate action or compulsive responses.
Evidence-Based Therapy Approaches
Exposure and Response Prevention (ERP)
ERP is the gold standard psychological treatment for OCD. This structured approach involves gradual exposure to situations that trigger obsessive thoughts while preventing the associated compulsive response. A trained therapist creates an exposure hierarchy customized for your specific OCD patterns. Sessions might involve imaginal exposure (visualizing feared scenarios) or in vivo exposure (real-life situations). The systematic nature of ERP helps your brain learn that intrusive thoughts are not dangerous, gradually reducing their frequency and intensity.
Cognitive Behavioral Therapy (CBT)
CBT for OCD targets the distorted thinking patterns that maintain the disorder. Therapists help you identify cognitive distortions like catastrophizing, overestimating threat probability, and inflated responsibility. Through structured exercises, you learn to challenge these patterns and develop more balanced perspectives. CBT also addresses the beliefs underlying OCD, such as the need for absolute certainty or perfect control, which fuel the obsessive-compulsive cycle.
Acceptance and Commitment Therapy (ACT)
ACT teaches psychological flexibility—the ability to experience uncomfortable thoughts and feelings without letting them control your behavior. Rather than trying to eliminate intrusive thoughts, ACT focuses on accepting their presence while committing to values-based actions. This approach particularly helps individuals who’ve become discouraged by traditional thought-stopping methods. ACT recognizes that attempting to suppress thoughts often increases their frequency, a phenomenon called the rebound effect.
Building Long-Term Resilience
Consistent daily practices strengthen your ability to manage OCD thoughts over time. Mindfulness meditation builds awareness of thought patterns without judgment. Regular physical exercise reduces baseline anxiety levels and improves overall mental health resilience. Adequate sleep supports prefrontal cortex function, which helps with impulse control and emotional regulation.
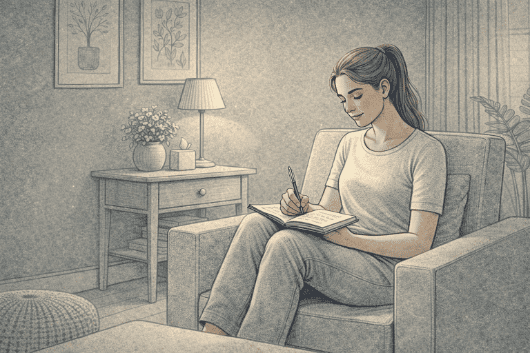
Maintaining a thought log helps identify patterns in your OCD symptoms. Track the situations that trigger intrusive thoughts, the content of those thoughts, your anxiety levels, and whether you performed compulsions. This data reveals trends that inform your treatment approach and demonstrates progress over time.
Support systems play a major role in OCD recovery. Whether through individual therapy, group therapy, or peer support communities, connecting with others who understand the experience reduces isolation and provides practical coping strategies. Family members and friends benefit from learning about OCD to provide appropriate support without inadvertently enabling compulsions.
Why A Mission For Michael Provides Expert OCD Treatment

A Mission For Michael’s residential and outpatient programs provide specialized OCD treatment using evidence-based therapies like ERP and CBT in comfortable, supportive environments across California, Virginia, and Washington.
At A Mission For Michael, we specialize in treating OCD and complex anxiety disorders through comprehensive evidence-based care. We maintain a 2:1 staff-to-client ratio, ensuring personalized attention throughout your treatment process.
Our programs integrate multiple therapeutic approaches, including EMDR for trauma-related OCD symptoms and holistic interventions like art therapy and mindfulness practices. We recognize that OCD often coexists with other mental health conditions, and our dual diagnosis expertise allows us to address the complete clinical picture. Treatment environments across our California, Virginia, and Washington locations provide comfortable, supportive spaces designed to facilitate healing.
Frequently Asked Questions (FAQs)
Can OCD thoughts ever completely go away?
With proper treatment, particularly ERP and CBT, most people experience a significant reduction in OCD thought frequency and intensity. Complete elimination isn’t always the goal. Instead, successful recovery means learning to experience intrusive thoughts without distress or compulsion.
Many individuals reach a point where occasional intrusive thoughts no longer interfere with daily functioning.
How long does it take for OCD treatment to work?
Most people notice improvement within 8 to 12 weeks of consistent ERP or CBT treatment, though timelines vary based on OCD severity and individual factors.
Residential or intensive outpatient programs can accelerate progress through daily therapy sessions. Sustained improvement requires ongoing practice of learned techniques even after formal treatment concludes.
Is it possible to manage OCD without medication?
Yes. Research demonstrates that psychological therapies like ERP and CBT effectively treat OCD without medication for many individuals. These approaches address the underlying thought patterns and behavioral cycles maintaining the disorder.
Some people benefit from combining therapy with medication, particularly those with severe symptoms or co-occurring conditions, but evidence-based therapy remains a cornerstone of effective OCD treatment.
What makes OCD different from regular worries or habits?
OCD thoughts are intrusive, unwanted, and cause significant distress, unlike normal worries, which people can typically set aside.
Compulsions in OCD feel necessary to prevent feared outcomes, whereas habits are performed willingly and don’t reduce anxiety. OCD significantly impairs daily functioning, relationships, or quality of life, distinguishing it from everyday concerns or preferences for routine.
What treatment approaches does A Mission For Michael use for OCD?
We provide comprehensive OCD treatment using evidence-based therapies, including Exposure and Response Prevention, Cognitive Behavioral Therapy, and Acceptance and Commitment Therapy. Our licensed clinical staff delivers these interventions through residential, PHP, IOP, and virtual outpatient programs with a 2:1 staff-to-client ratio.
We also integrate holistic approaches and specialize in treating OCD alongside co-occurring mental health conditions for complete, personalized care. A Mission For Michael offers comprehensive therapeutic support customized for your needs.