Key Takeaways
- OCD brains show structural and functional differences, particularly in regions such as the orbitofrontal cortex, basal ganglia, and anterior cingulate cortex, which drive persistent doubt and compulsive behaviors.
- Hyperactive error detection and altered CSTC circuits make intrusive thoughts feel significant, creating obsessions and anxiety that are hard to dismiss.
- Compulsions develop because behaviors temporarily reduce anxiety, reinforcing neural pathways and making rituals automatic over time.
- Neurotransmitter imbalances in serotonin, glutamate, and dopamine interact with structural differences, influencing intrusive thoughts, compulsions, and the overall anxiety-compulsion cycle.
- At A Mission For Michael (AMFM), we combine evidence-based therapies, personalized treatment plans, and compassionate support to help clients retrain neural pathways, reduce OCD symptoms, and build lasting mental wellness.
The Differences Between OCD & Typical Brain Function
The OCD brain isn’t just thinking differently—it shows structural and functional distinctions from a typical brain. These differences aren’t visible without advanced neuroimaging, which reveals consistent patterns across interconnected regions that process information and regulate behavior in unique ways.
OCD primarily involves disruptions in error detection and threat assessment. While a typical brain filters out false alarms, an OCD brain flags normal thoughts as dangerous and struggles to recognize when a threat is resolved. This drives the characteristic “doubt loop,” where repeated checking, cleaning, or other behaviors occur because the brain doesn’t signal completion or safety.
Founded in 2010, A Mission For Michael (AMFM) offers specialized mental health care across California, Minnesota, and Virginia. Our accredited facilities provide residential and outpatient programs, utilizing evidence-based therapies such as CBT, DBT, and EMDR.
Our dedicated team of licensed professionals ensures every client receives the best care possible, supported by accreditation from The Joint Commission. We are committed to safety and personalized treatment plans.
Brain Structure Differences in OCD
Neuroimaging shows subtle structural differences in key brain regions of people with OCD, including the orbitofrontal cortex, basal ganglia, anterior cingulate cortex, and thalamus. These variations in size, density, and connectivity aren’t damage but influence decision-making, habit formation, and behavior regulation.
Differences among individuals help explain diverse symptom patterns and highlight the need for personalized treatment. Importantly, successful therapy can normalize some structural and functional changes, showing the brain’s adaptability.
Abnormal Activity in the Orbitofrontal Cortex
The orbitofrontal cortex (OFC) is hyperactive in OCD, affecting decision-making and emotional regulation. This overactivity makes it hard to feel “done” with tasks and exaggerates the significance of normal thoughts. Altered connectivity with other regions reinforces persistent doubt, which can normalize with effective treatment.
Basal Ganglia Size & Function Changes
The basal ganglia, especially the caudate nucleus, show structural and functional differences in OCD. These “automatic transmission” structures help regulate routine behaviors, and when impaired, the brain gets “stuck” in repetitive thought or actions, explaining OCD compulsions.
Altered Connections in the CSTC Circuit
The cortico-striato-thalamo-cortical (CSTC) circuit forms a feedback loop for evaluating actions and thoughts. In OCD, hyperactivity and altered connectivity trap the brain in doubt loops, perpetuating compulsive behaviors.
Temporary relief from compulsions reinforces the cycle at the brain-circuit level.
Brain Chemistry Differences in OCD
Beyond structural differences, the OCD brain shows distinct variations in neurotransmitter systems, the chemical messengers that allow brain cells to communicate.
These chemical differences interact with structural abnormalities in regions such as the orbitofrontal cortex and the basal ganglia, shaping how thoughts and behaviors are processed. Understanding these interactions helps explain why specific treatments work better for some individuals than others.
Serotonin Imbalances
Serotonin, beyond regulating mood, also affects threat assessment and the sense of action completion. Dysregulation contributes to heightened anxiety, intrusive thoughts, and compulsive behaviors. SSRIs often help normalize CSTC circuit activity, reducing obsessions and the urge to perform rituals, usually at higher doses than used for depression.
Glutamate Dysregulation
Excess glutamate or abnormal receptor sensitivity causes neural hyperactivity, reinforcing the “stuck in gear” feeling common in OCD. A study used magnetic resonance spectroscopy (MRS) to examine GABA and glutamate in the anterior cingulate cortex of adults with OCD.
Results showed higher GABA levels and an increased GABA-to-glutamate ratio in OCD patients, while glutamate alone did not differ. Findings suggest that an imbalance between GABA and glutamate, rather than glutamate abnormalities alone, plays a key role in OCD pathophysiology.
Dopamine & Compulsive Behaviors
Dopamine dysfunction, especially in the striatum, reinforces compulsions by giving faulty reward feedback. In some cases, dopamine-modulating medications help break these reinforcement loops, particularly for “just-right” compulsions or comorbid tic disorders.
What Brain Scans Actually Show in OCD Patients
Modern neuroimaging techniques have revolutionized our understanding of the OCD brain, showing both structural and functional differences in living individuals. MRI, fMRI, PET, and similar tools consistently reveal patterns of abnormality, confirming OCD has clear neurobiological underpinnings.
However, these scans are research tools, not diagnostic methods, and findings reflect group averages rather than definitive markers in any single person.
PET Scan Findings & What They Mean
PET scans measure metabolic activity by tracking glucose use, revealing hyperactivity in the orbitofrontal cortex, anterior cingulate cortex, and caudate nucleus. These overactive regions align with the CSTC circuit involved in OCD. Successful treatment often normalizes these patterns, linking symptom improvement directly to changes in brain activity.
fMRI Evidence of Altered Brain Activity
fMRI shows heightened activity in error-detection circuits when patients face triggers. fMRI research shows amygdala hyperactivation as a common neural correlate in OCD, which can be dampened through attentional distraction during symptom provocation. For example, those with contamination fears may show exaggerated responses to images of germs, and neural activity may correlate with obsessions and compulsions.
Limitations of Using Brain Scans for Diagnosis
Scans cannot reliably diagnose OCD. Differences reflect averages, overlap with other conditions, and are subtle, often appearing normal to the untrained eye. Clinical assessment remains the gold standard.
The Error Detection System Gone Wrong
OCD involves a hyperactive error detection system, the brain network that flags potential problems. In a typical brain, this system activates in response to genuine errors, resolves the issue, and returns to baseline.
In OCD, it remains overly sensitive and struggles to “turn off,” creating persistent doubt and the feeling that something is incomplete. This explains why reassurance and logical reasoning often fail to alleviate symptoms.
How Normal Brains Process Doubt & Certainty
In neurotypical brains, certainty comes from multiple regions working together. Sensory feedback, memory, and emotion are integrated, while the anterior cingulate cortex checks for errors. When no errors are detected, the prefrontal cortex signals completion, allowing people to move on without doubt.
Why the OCD Brain Gets Stuck in Doubt Loops
In OCD, the anterior cingulate cortex continues to signal potential errors, while the orbitofrontal cortex fails to register “all clear.” The result is persistent doubt that isn’t resolved by logic or memory, driving repeated checking and reassurance-seeking.
The Anxiety-Compulsion Cycle in the Brain
Obsessions trigger the amygdala, raising anxiety and activating hyperactive orbitofrontal and anterior cingulate regions. Compulsions temporarily reduce this anxiety and activate the reward system, reinforcing the behavior. Over time, this strengthens automatic neural pathways, making the cycle difficult to break and requiring repeated effort to form new patterns.
How These Brain Differences Create OCD Symptoms
Structural and functional brain differences in OCD interact to produce characteristic symptoms. Obsessions arise from hyperactive thought-generating regions combined with poor filtering mechanisms that would normally dismiss intrusive thoughts.
Compulsions develop because the brain’s reward and habit systems learn that these behaviors temporarily reduce distress, making the cycle feel compelling despite being recognized as irrational.
Different Symptom Presentations
Variations in affected neural pathways help explain different OCD symptoms, such as checking, contamination fears, symmetry needs, or forbidden thoughts, and why treatments often need to be specific to symptom types. Neurobiological differences influence both the development and manifestation of OCD.
From Brain Activity to Intrusive Thoughts
Intrusive thoughts occur in most people, but the OCD brain flags them as significant or dangerous. Hyperactivity in the anterior cingulate cortex and orbitofrontal cortex, combined with amygdala-driven fear responses, transforms fleeting thoughts into obsessions that generate real distress.
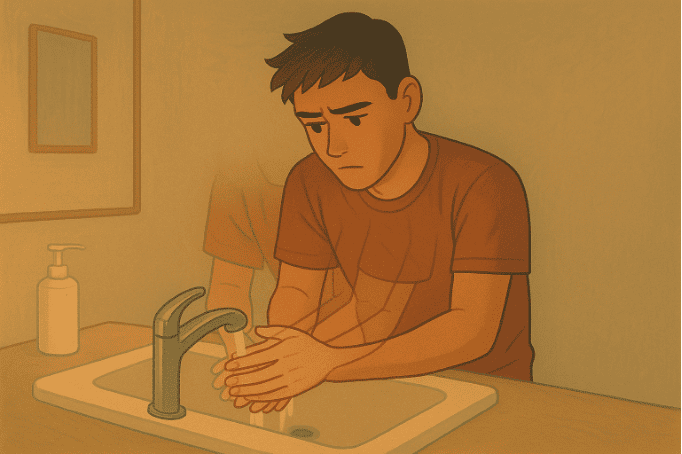
The Neurological Basis of Compulsive Rituals
Compulsions are reinforced when behaviors reduce anxiety, strengthening neural pathways in the basal ganglia and making rituals increasingly automatic. Altered sequence-monitoring systems explain why actions must often be performed in precise ways to feel “right.”
Why Reassurance Seeking Doesn’t Work
Reassurance provides temporary relief but fails to correct the dysfunctional error detection system. Repeated reassurance strengthens doubt pathways, making OCD more entrenched and highlighting the need for treatment strategies that develop internal assessment mechanisms.
Treatment Approaches Based on Brain Science
Effective therapy rewires neural circuits, reducing OCD-driven fear responses.
Understanding the brain differences in OCD has helped shape targeted, effective treatments. Modern interventions focus on the circuits and pathways maintaining the disorder, creating lasting change rather than just addressing symptoms.
Deep Brain Stimulation (DBS): When and How It Works
For severe, treatment-resistant OCD, DBS modulates key brain regions in the CSTC circuit using targeted electrical impulses. This approach can help reset overactive circuits when other therapies alone aren’t enough.
A 12-month study shows that DBS targeting the Bed Nucleus of Stria Terminalis (BNST) improves symptoms and cognitive flexibility in treatment-resistant OCD with minimal side effects.
How CBT Physically Rewires Neural Pathways
Cognitive-Behavioral Therapy (CBT) is highly effective because it reshapes neural circuits through neuroplasticity. Facing fears without performing compulsions strengthens healthier pathways while weakening the old, dysfunctional ones.
A study shows that 12 weeks of CBT for OCD can normalize brain network connectivity, directly linking changes in neural circuits to symptom improvement.
Behavioral & Experiential Therapies
Therapies that combine CBT with real-life exercises, mindfulness, and anxiety-management strategies help retrain the brain’s error detection system. By practicing new coping skills in safe, guided settings, patients reduce compulsive behaviors and improve daily functioning.
Integrated, Personalized Treatment
Tailoring therapy plans to each individual’s symptoms and brain patterns maximizes recovery. Combining CBT, behavioral strategies, and supportive care helps break compulsive cycles, reduce anxiety, and build lasting mental wellness.
OCD Brain vs Normal Brain: Comparison Table
| Brain Feature | Typical Brain | OCD Brain |
| Orbitofrontal Cortex (OFC) | Normal activity levels; helps with decision-making and recognizing task completion | Hyperactive; struggles to signal “done,” exaggerates the significance of everyday thoughts |
| Basal Ganglia (Caudate Nucleus) | Regulates routine behaviors smoothly; acts as “automatic transmission” | Structural and functional differences; the brain gets “stuck” in repetitive thoughts or actions |
| Anterior Cingulate Cortex | Detects genuine errors, then returns to baseline | Persistently signals potential errors even when none exist; creates doubt loops |
| CSTC Circuit | Balanced feedback loop for evaluating actions and thoughts | Hyperactive with altered connectivity; traps the brain in persistent doubt loops |
| Error Detection System | Flags real problems, resolves them, then turns off | Overly sensitive; remains activated and struggles to “turn off,” creating persistent doubt |
| Doubt & Certainty Processing | Integrates sensory feedback, memory, and emotion; signals completion without lingering doubt | Anterior cingulate keeps signaling errors; OFC fails to register “all clear”; persistent doubt remains |
| Serotonin Levels | Balanced regulation of mood, threat assessment, and action completion | Dysregulated; contributes to heightened anxiety, intrusive thoughts, and compulsive behaviors |
| Glutamate System | Normal levels and receptor sensitivity | Excess glutamate or abnormal sensitivity; causes neural hyperactivity and “stuck in gear” feeling |
| Dopamine Function | Provides accurate reward feedback for behaviors | Dysfunction in striatum; gives faulty reward feedback, reinforcing compulsions |
| GABA-to-Glutamate Ratio | Balanced ratio supporting normal neural function | Elevated GABA levels and increased GABA-to-glutamate ratio; contributes to OCD pathophysiology |
| Intrusive Thoughts | Occur briefly but are easily dismissed as unimportant | Flagged as significant or dangerous; transformed into distressing obsessions |
| Anxiety-Compulsion Cycle | Temporary anxiety is resolved without ritualistic behaviors | Obsessions trigger amygdala, raising anxiety; compulsions provide temporary relief, reinforcing the cycle |
| Compulsive Behaviors | Not needed; brain signals task completion naturally | Become automatic through reinforced neural pathways; must be performed in precise ways to feel “right” |
| Response to Reassurance | Accepts reassurance and moves on | Temporary relief only; reassurance strengthens doubt pathways and makes OCD more entrenched |
| Brain Scan Activity (PET) | Normal metabolic activity in decision-making regions | Hyperactivity in orbitofrontal cortex, anterior cingulate cortex, and caudate nucleus |
| Brain Scan Activity (fMRI) | Normal error-detection circuit activation | Heightened activity in error-detection circuits; exaggerated responses to triggers |
| Treatment Response | Not applicable | Brain activity can normalize with effective treatment (CBT, ERP, medication); demonstrates neuroplasticity |
AMFM: Supporting OCD Recovery Together
At A Mission for Michael (AMFM), we understand that OCD is rooted in fundamental brain differences, both structural and chemical. That’s why our approach combines evidence-based therapies and compassionate support to address the underlying neurobiology of obsessive-compulsive behaviors.

Guidance at AMFM helps clients break long-standing fear loops with structured, evidence-based care.
Personalized Treatment for Lasting Change
We know that OCD symptoms vary from person to person. Our team creates tailored treatment plans that reflect each client’s unique patterns of brain activity and behavior. By addressing obsessions, compulsions, and the anxiety-compulsion cycle, we help clients retrain their neural pathways toward healthier responses.
Integrated Therapy & Support
Our programs combine CBT, Exposure and Response Prevention (ERP), family support, and, when appropriate, medication management. We focus on both the mind and the brain, helping clients develop skills that translate into real-world confidence and control over OCD symptoms.
Compassionate, Evidence-Based Care
We go beyond generic treatment formulas. We see the person behind the diagnosis and guide them with empathy and expertise, helping them process the challenges created by hyperactive error detection, doubt loops, and compulsive behaviors.
Accessible & Supportive Process
From your first call to ongoing care, we provide guidance every step of the way. Our team helps with insurance navigation, personalized assessments, and continuous monitoring to ensure each client’s treatment remains effective and responsive to progress.
Transforming Lives with Science & Compassion
At AMFM, we believe OCD can be managed because the brain is adaptable. By combining neurobiological insights with compassionate care, we empower clients to break cycles, reduce distress, and build lasting mental wellness.
Frequently Asked Questions (FAQs)
Is OCD a structural brain disorder or a chemical imbalance?
OCD involves both structural and chemical brain differences. Altered regions like the orbitofrontal cortex and basal ganglia interact with neurotransmitter imbalances (serotonin, dopamine, glutamate), explaining why combined treatments, medication, and psychotherapy effectively target symptoms through neuroplasticity.
Can doctors diagnose OCD using brain scans alone?
No. Brain scans reveal group-level patterns but aren’t reliable for individual diagnosis. Differences overlap with normal variation and other conditions. Clinical assessment of symptoms, impact, and consistency with diagnostic criteria remains the gold standard.
Does having these brain differences mean OCD can’t be treated effectively?
Not at all. OCD brain differences are modifiable. Treatment via medication, therapy, or both normalizes brain activity, reduces symptoms, and uses neural plasticity. Even severe or resistant cases can respond to advanced interventions such as deep-brain stimulation.
Can therapy change OCD brain patterns?
Yes. Evidence-based therapies such as ERP or CBT can help retrain neural pathways. At AMFM, we provide these therapies in a supportive, personalized setting, assisting clients to reduce OCD hyperactivity and strengthen healthier brain responses over time.
Are children with OCD affected in the same way as adults?
Children show similar brain differences, particularly in the orbitofrontal cortex and basal ganglia, but these patterns may vary with brain development. Early intervention supports neural adaptation and long-term symptom improvement.