Key Takeaways
- Up to 50% of people with Borderline Personality Disorder (BPD) experience psychotic symptoms like hallucinations and paranoid thoughts.
- BPD-related psychosis typically differs from other psychotic disorders as symptoms are usually brief, stress-triggered, and the person often maintains some reality testing.
- Psychotic symptoms in BPD can include paranoia, auditory hallucinations, visual distortions, and severe dissociative episodes.
- Relationship conflicts and abandonment fears commonly trigger psychotic episodes in people with BPD.
- A Mission For Michael (AMFM) employs comprehensive treatment approaches, including Dialectical Behavior Therapy (DBT) and sometimes carefully prescribed medications for BPD symptom management.
The Complex Relationship Between BPD and Psychosis
Borderline Personality Disorder (BPD) is primarily characterized by emotional dysregulation, unstable relationships, identity disturbances, and impulsivity. Psychosis, on the other hand, involves a disconnect from reality that may include hallucinations or delusions. While these are distinct mental health phenomena, they can overlap in complex ways in people with BPD.
Research indicates that stress-related psychotic symptoms occur in approximately up to 50% of individuals with BPD. These episodes are typically brief, lasting hours to days rather than weeks or months, as seen in primary psychotic disorders like schizophrenia.
The psychotic symptoms in BPD are often described as “micro-psychotic” episodes that are triggered by interpersonal stressors or abandonment fears. Unlike in primary psychotic disorders, individuals with BPD often maintain some awareness that their perceptions may not reflect objective reality.
Founded in 2010, A Mission For Michael (AMFM) offers specialized mental health care across California, Minnesota, and Virginia. Our accredited facilities provide residential and outpatient programs, utilizing evidence-based therapies such as CBT, DBT, and EMDR.
Our dedicated team of licensed professionals ensures every client receives the best care possible, supported by accreditation from The Joint Commission. We are committed to safety and personalized treatment plans.
What Psychotic Symptoms Look Like in BPD
Psychotic symptoms in BPD can manifest in various ways, but they commonly emerge during periods of intense emotional distress.
Stress-Triggered Paranoid Thoughts
People with BPD often experience paranoid ideation during times of heightened stress or perceived rejection. These thoughts typically center around themes of persecution, betrayal, or abandonment by significant others.
For example, a person with BPD might become convinced that their partner is secretly planning to leave them based on minimal or misinterpreted evidence, such as a delayed text response or a neutral facial expression.
Unlike the fixed delusions seen in schizophrenia, paranoid thoughts in BPD are usually transient and directly connected to emotional triggers. They tend to intensify during interpersonal conflicts and may diminish when the individual receives reassurance or when the emotional crisis passes. This fluctuating nature is characteristic of BPD-related paranoia.
Auditory Hallucinations
Auditory hallucinations are among the most common psychotic symptoms experienced by people with BPD. These hallucinations often take the form of critical or derogatory voices that reinforce negative self-beliefs and can be highly distressing.
Unlike the auditory hallucinations in schizophrenia, which may be bizarre or completely detached from reality, BPD-related voices frequently echo the person’s own thoughts about themselves.
They might hear phrases like “you’re worthless,” “nobody will ever love you,” or “you should hurt yourself,” internal criticisms externalized as auditory experiences. These hallucinations typically emerge during periods of isolation, stress, or emotional dysregulation.
Dissociative Experiences
Dissociation in BPD can sometimes reach psychotic-like intensity, creating significant distortions in how people perceive themselves and their environment. Severe dissociative episodes may involve feeling completely detached from reality, experiencing the world as dreamlike or unreal (derealization), or feeling disconnected from one’s body or sense of self (depersonalization).
During intense dissociative states, individuals may report feeling like they’re observing themselves from outside their body, that the world around them isn’t real, or that familiar environments suddenly seem strange or threatening. These experiences, while not technically classified as psychosis, can significantly impair reality testing and create frightening distortions in perception.
How BPD Psychosis Differs from Other Psychotic Disorders
Duration and Intensity of Symptoms
The psychotic symptoms experienced in BPD are typically briefer and more situational than those seen in disorders like schizophrenia or schizoaffective disorder.
The intensity of symptoms also fluctuates more rapidly in BPD. A person might appear completely in touch with reality during a therapy session, only to experience significant psychotic symptoms hours later following a relationship conflict.
This pattern of rapid fluctuation is much less common in primary psychotic disorders, where symptoms tend to develop and resolve more gradually and follow a less predictable course in relation to external stressors.
Awareness of Reality
People experiencing BPD-related psychosis often maintain some level of insight or awareness that their perceptions may be distorted, even during acute episodes. They might describe feeling “crazy” or recognize afterward that their perceptions were influenced by emotional distress.
This partial insight contrasts with primary psychotic disorders, where individuals typically lack awareness that their hallucinations or delusions are not objectively real, making them less likely to question these experiences even after the acute phase has passed.
Triggers and Patterns
The psychotic symptoms in BPD are consistently triggered by specific types of situations, particularly those involving perceived abandonment, rejection, or criticism.
This predictable pattern differs from primary psychotic disorders, where episodes may occur without clear environmental triggers or may be precipitated by a wider range of stressors not specifically related to interpersonal relationships.
Illustrative Examples of BPD Psychotic Episodes
Relationship Abandonment Triggers
Jamie experienced her first psychotic episode after her partner mentioned needing to work late several nights in a row. What began as typical BPD abandonment fear quickly escalated: she became convinced her partner was having an affair and lying about work commitments.
Despite no evidence, Jamie began hearing whispered conversations when alone in her apartment and believed she could hear her partner’s voice discussing plans to leave her. She checked her partner’s phone repeatedly, seeing “coded messages” in ordinary texts. When her partner finally came home and spent quality time with her, the voices and paranoid beliefs gradually subsided over 24 hours.
Stress-Induced Paranoia Scenarios
After receiving minor criticism during a work performance review, Alex, with BPD, developed the belief that his coworkers were conspiring to get him fired. He began misinterpreting casual conversations, believing colleagues were speaking in code about him.
He perceived threatening messages in ordinary emails and felt certain the office security cameras were specifically monitoring his movements. When alone at his desk, he heard faint voices discussing his “failures” and “replacement.” This paranoid episode lasted approximately three days, during which Alex nearly quit his job. After using crisis management skills learned in therapy and taking a mental health day, his thinking gradually cleared.
These examples highlight several important features of BPD psychosis: the clear emotional trigger, the content reflecting core BPD fears (abandonment, rejection), the brief duration, and the resolution once emotional distress decreased.
Unlike psychosis in schizophrenia, these episodes didn’t require antipsychotic medication to resolve, though medication may sometimes be helpful for symptom management.
Effective Treatment Approaches for BPD with Psychotic Features
Dialectical Behavior Therapy (DBT)
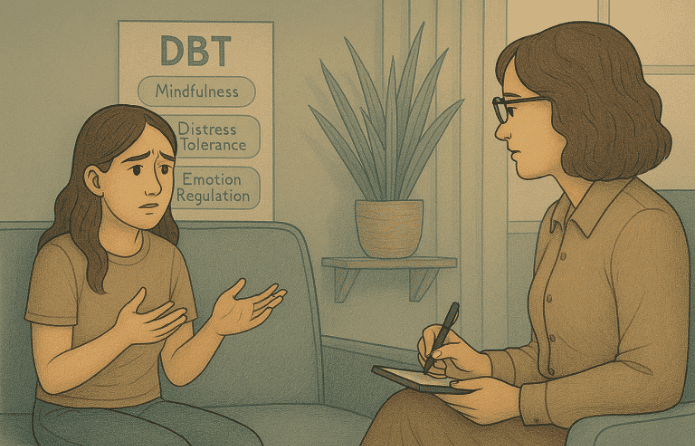
DBT remains the gold standard treatment for BPD and shows effectiveness for BPD with psychotic features.
DBT teaches specific skills for emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness, all crucial for preventing the emotional escalations that trigger psychotic episodes. The therapy’s emphasis on building a life worth living helps address the emptiness and instability that characterize BPD.
For managing psychotic symptoms specifically, DBT offers reality testing skills and grounding techniques that help individuals anchor themselves during perceptual disturbances. The “check the facts” skill is particularly valuable for addressing paranoid thinking, while mindfulness practices help people distinguish between thoughts, emotions, and objective reality.
Medication Options and Considerations
Medication approaches for BPD with psychotic features remain somewhat controversial, as research specifically targeting this presentation is limited. Low-dose atypical antipsychotics are sometimes prescribed to reduce the intensity of psychotic symptoms and help with emotional regulation.
However, these medications are generally used at lower doses than would be prescribed for schizophrenia, and the focus remains on psychotherapy as the primary treatment.
Crisis Management Strategies
For individuals with BPD who experience psychotic symptoms, having a crisis management plan is essential. These plans should be developed collaboratively with mental health professionals and outline specific steps to take when psychotic symptoms emerge.
Effective plans typically include early warning signs, grounding techniques, contact information for support people, and clear guidelines about when to seek emergency care.
Understanding BPD Psychosis: Comprehensive Treatment at AMFM
At AMFM, we recognize that BPD with psychotic features demands expert care combining evidence-based psychotherapy with compassionate, round-the-clock support. Our residential treatment programs specialize in treating the complex intersection of emotional instability and psychotic symptoms through comprehensive Dialectical Behavior Therapy, the gold standard for BPD treatment.
Our experienced clinicians help individuals develop crucial skills in emotional regulation, distress tolerance, reality testing, and crisis management, tools essential for preventing and managing psychotic episodes.

AMFM’s structured residential environments across California, Minnesota, and Virginia provide the intensive support needed during acute phases while building long-term resilience.
We combine individual therapy, group interventions, family support, and, when appropriate, carefully managed medication, all within safe, nurturing settings designed for healing. Whether you’re experiencing your first psychotic episode or struggling with recurring symptoms, AMFM’s multidisciplinary approach addresses both the emotional triggers and the psychotic experiences themselves. Contact us today to learn how our specialized BPD treatment programs can help you achieve lasting stability and recovery.
Frequently Asked Questions
Can BPD psychotic episodes happen without obvious triggers?
While most BPD-related psychotic episodes have clear emotional triggers like perceived abandonment or rejection, sometimes the trigger may not be immediately obvious to observers. The person with BPD might be experiencing internal emotional distress that others don’t recognize. Additionally, accumulated stress from multiple smaller events can eventually trigger psychotic symptoms even when no single dramatic event occurred.
How long do psychotic episodes typically last in BPD?
BPD-related psychotic episodes typically last hours to days rather than weeks or months, as seen in primary psychotic disorders. Most episodes resolve within 24–72 hours once the emotional crisis passes or the person receives support and uses coping skills. This brief duration distinguishes BPD psychosis from schizophrenia, where episodes persist much longer.
Can someone with BPD completely avoid psychotic episodes?
With proper treatment, including DBT, emotional regulation skills, and crisis management strategies, many people with BPD significantly reduce the frequency and intensity of psychotic episodes. While complete prevention may not be guaranteed for everyone, comprehensive treatment helps individuals recognize early warning signs, manage triggers effectively, and intervene before symptoms escalate to full psychosis.
How does AMFM treat BPD with psychotic features?
AMFM offers specialized residential programs combining Dialectical Behavior Therapy, individual and group counseling, crisis management training, and medication management when appropriate. Our multidisciplinary teams provide 24/7 support in structured environments designed to help individuals develop emotional regulation skills, reality testing abilities, and effective coping strategies for managing both BPD symptoms and psychotic experiences.