Key Takeaways
- Between 50% and 98% of people with schizophrenia experience anosognosia, a neurological symptom that prevents them from recognizing they have a mental health condition.
- Self-awareness in schizophrenia exists on a spectrum—some people have partial insight while others have none at all.
- Lack of awareness isn’t stubbornness or denial but a genuine symptom caused by changes in brain function.
- Treatment can improve self-awareness over time, allowing many people to recognize their symptoms.
- A Mission for Michael (AMFM) offers specialized residential treatment programs for schizophrenia with 24/7 care, evidence-based therapies like CBT, medication management, and compassionate support designed to help individuals regain stability even when insight is limited.
Many People With Schizophrenia Don’t Recognize Their Symptoms
Research consistently shows that approximately 50%–98% of people with schizophrenia have limited or no awareness that they’re experiencing a mental health condition. This neurological symptom, which prevents recognition of illness, is one of the most challenging aspects of schizophrenia for both those living with the condition and their support networks.
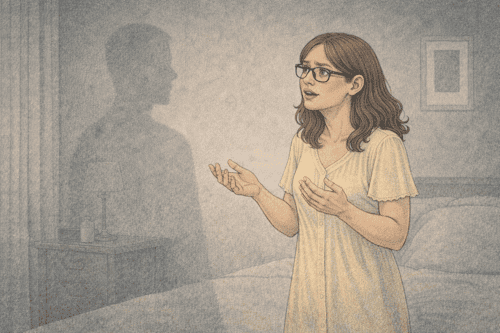
During active psychosis, a person with schizophrenia may be utterly convinced that their hallucinations and delusions reflect reality. They might hear voices and genuinely believe others can hear them, too. Or they might develop complex belief systems about being persecuted or having special powers that seem entirely factual to them.
These symptoms feel as real as any other sensory experience. Even when confronted with evidence that contradicts their perceptions, many people with schizophrenia cannot incorporate this information into their understanding. The disconnection between their experiences and what others tell them can lead to frustration, isolation, and resistance to treatment.
What is Anosognosia?
Anosognosia is the medical term for lack of insight or unawareness of illness. Unlike simple denial, which is a psychological defense mechanism, anosognosia in schizophrenia is a neurological symptom caused by physical changes in brain function.
The frontal and parietal lobes, which help us develop accurate self-awareness, don’t function properly, making it impossible for the person to recognize their condition.
This isn’t stubbornness or willful ignorance. The brain literally cannot see what’s happening to itself, similar to how someone with certain types of stroke damage might not recognize paralysis on one side of their body.
Founded in 2010, A Mission For Michael (AMFM) offers specialized mental health care across California, Minnesota, and Virginia. Our accredited facilities provide residential and outpatient programs, utilizing evidence-based therapies such as CBT, DBT, and EMDR.
Our dedicated team of licensed professionals ensures every client receives the best care possible, supported by accreditation from The Joint Commission. We are committed to safety and personalized treatment plans.
How Schizophrenia Affects Self-Awareness
The Spectrum of Insight: It’s Not All or Nothing
Self-awareness in schizophrenia exists on a spectrum rather than being completely present or absent. Some people have momentary flashes of insight in which they recognize that something unusual is happening, while others maintain awareness of specific symptoms but not others.
For example, someone might acknowledge hearing voices but insist they come from real people monitoring them, not from their own mind. Insight can also fluctuate over time and with treatment.
During periods of symptom remission or with effective medication, many people gain greater awareness of their condition. Some describe this experience as “waking up” or suddenly seeing their experiences from a new perspective.
This fluctuating awareness creates complex challenges, as a person might accept treatment during periods of clarity but reject it when symptoms intensify and insight diminishes.
Why the Brain Can’t Recognize Its Own Symptoms
The inability to recognize symptoms in schizophrenia stems from disruptions in neural pathways that connect different regions of the brain. When these communication highways malfunction, the brain cannot properly integrate information about itself.
Neuroimaging studies have shown reduced connectivity between the frontal lobes (responsible for executive functioning and self-assessment) and other brain regions in people with limited insight into their schizophrenia.
This neurological basis explains why simply explaining to someone that they have schizophrenia often doesn’t change their perspective. The very circuits needed to process and accept this information aren’t functioning correctly.
Additionally, the brain naturally tries to make sense of unusual experiences, leading people with schizophrenia to develop explanations that seem more plausible to them than mental illness.
Signs Someone May Not Know They Have Schizophrenia
Schizophrenia often affects insight, making it difficult for someone to recognize their own symptoms.
Recognizing when someone lacks insight into their condition can help family members better understand their loved one’s perspective and approach the situation more effectively.
1. Consistently Denying Symptoms Despite Evidence
When someone consistently denies having any symptoms despite clear evidence to the contrary, it often indicates anosognosia rather than deliberate deception. They may insist they don’t hear voices even when observed responding to them, or deny having paranoia despite expressing elaborate conspiracy theories.
This denial persists even when presented with concrete evidence like recordings of their behavior during psychotic episodes or testimonies from multiple witnesses.
2. Attributing Symptoms to External Forces
People who lack insight into schizophrenia typically attribute their symptoms to external causes rather than recognizing them as coming from their own mind.
Hallucinated voices become real people speaking to them, perhaps through special technology or supernatural means. Thought disturbances might be blamed on external interference, such as government mind control or alien communication.
These external attributions often follow logical patterns based on the person’s experiences and cultural background. Someone with technical knowledge might develop elaborate theories about surveillance technology, while someone with religious beliefs might interpret symptoms as spiritual communications.
3. Resistance to Treatment or Medication
One of the most challenging aspects of anosognosia is that it often leads to treatment refusal. From the perspective of someone who doesn’t believe they have an illness, medications seem unnecessary at best and potentially harmful at worst.
They may view suggestions to take antipsychotics as attempts to control them, especially if they believe others are conspiring against them. This creates a problematic situation in which the very treatment that could help restore insight is rejected precisely because of a lack of understanding.
4. Lack of Recognition of Behavior Changes
People experiencing anosognosia often cannot recognize significant changes in their own behavior, thinking, or functioning. They might have gone from being organized and articulate to speaking in jumbled sentences and being unable to maintain basic self-care, yet they perceive no difference in themselves.
This inability to recognize changes extends to both positive symptoms (like hallucinations) and negative symptoms (like social withdrawal or diminished emotional expression).
When People With Schizophrenia Do Recognize Their Condition

Despite the prevalence of anosognosia in schizophrenia, many people do develop awareness of their condition, especially over time and with effective treatment.
Factors That Improve Self-Awareness
Several therapeutic approaches have proven effective in helping people with schizophrenia develop insight into their condition, even without medication as the primary intervention. Cognitive Behavioral Therapy (CBT) for psychosis specifically addresses beliefs and experiences in a non-confrontational way, helping individuals explore alternative explanations for their symptoms. Through this process, many people gradually develop the ability to question whether their perceptions might be symptoms rather than reality.
Peer support programs provide invaluable opportunities to learn from others with similar experiences. Connecting with people who have successfully managed schizophrenia helps normalize the condition and demonstrates that recovery is possible. These relationships often create openings for self-awareness that professional interventions alone cannot achieve.
Therapeutic relationships built on trust and consistency play a crucial role in developing insight over time. When clinicians validate emotional experiences while gently introducing alternative perspectives, individuals feel safe enough to consider that their symptoms might stem from a treatable condition rather than external forces. Family therapy and psychoeducation also help both individuals and their support systems understand the neurological basis of anosognosia, reducing conflict and improving engagement with treatment.
Psychosocial interventions, including social skills training and supported employment programs, help people recognize improvements in their functioning, which can indirectly build awareness. When someone experiences concrete benefits from participating in structured therapeutic activities—better relationships, increased independence, improved daily functioning—they often become more open to understanding what was interfering with these areas previously.
How Integrated Treatment Approaches Support Recovery
The most effective path to improving insight combines multiple therapeutic modalities tailored to each individual’s needs and current level of awareness. CBT for psychosis helps people examine their beliefs without requiring them to immediately accept that they have schizophrenia. Instead, therapists work collaboratively to identify patterns, explore evidence, and develop coping strategies that work regardless of what someone believes about their symptoms.
Supportive psychotherapy creates a safe space for processing confusing experiences and building the therapeutic alliance necessary for long-term engagement. Many people who initially reject the diagnosis of schizophrenia will participate in therapy focused on stress management, relationship difficulties, or other concerns they do recognize—and through this engagement, gradually develop broader awareness.
For some individuals, medication becomes a helpful complementary tool alongside these therapeutic approaches. Antipsychotic medications can help normalize brain function, particularly in the prefrontal cortex, which may support the neurological pathways involved in self-awareness. When medications reduce symptom intensity, many people find they can more easily engage with psychological therapies and begin questioning their previous certainties. However, meaningful recovery and improved insight are possible through consistent therapeutic engagement, supportive relationships, and structured psychosocial interventions, with medication serving as one potential support rather than the sole solution.
Supporting Self-Awareness & Recovery With AMFM
When someone with schizophrenia doesn’t recognize their condition, getting them the help they need requires specialized expertise and extraordinary patience. At A Mission for Michael (AMFM), we understand that lack of insight isn’t defiance—it’s a neurological symptom that requires compassionate, strategic care.

Our residential treatment programs are designed to engage individuals with schizophrenia regardless of their current level of self-awareness.
We focus on building trust, addressing the concerns your loved one recognizes, and providing comprehensive therapeutic interventions that can gradually restore insight. Our experienced clinical team specializes in Cognitive Behavioral Therapy for psychosis, supportive psychotherapy, peer support programming, and family therapy—all designed to work with anosognosia rather than against it.
These evidence-based therapies help individuals explore their experiences in a non-threatening way, develop coping strategies, and build the self-awareness necessary for long-term recovery. We create individualized treatment plans that meet people where they are, validating their emotional reality while gently introducing alternative perspectives. For those who may benefit, we also provide medication management as a complementary support to enhance the effectiveness of therapeutic interventions.
With 24/7 professional support at our Washington, California, Virginia, and Minnesota locations, we provide the structured, safe environment needed for stabilization and recovery. Our comprehensive approach includes daily living skills training, experiential therapies, and ongoing support that continues even after residential treatment ends.
You don’t have to manage this challenging journey alone. Contact AMFM to learn how our therapeutic programs can help your loved one move toward stability and greater self-understanding.
Frequently Asked Questions (FAQs)
Is the lack of awareness in schizophrenia the same as denial?
No, anosognosia differs fundamentally from psychological denial. Denial is a defense mechanism where someone unconsciously rejects painful realities they’re capable of perceiving. Anosognosia results from a neurological impairment that prevents the brain from accurately monitoring its own state.
Neuroimaging studies show actual differences in brain function, particularly in prefrontal and parietal regions. This distinction matters because therapeutic approaches must address the underlying neurological factors while building awareness through evidence-based psychological interventions like CBT for psychosis, which can help restore insight over time.
Can someone with schizophrenia eventually develop self-awareness?
Yes, many people develop significant insight with consistent treatment over time. This process typically occurs gradually through engagement with evidence-based therapies, peer support, and psychosocial interventions, with periods of partial awareness before fuller understanding emerges.
CBT for psychosis helps individuals examine their beliefs and experiences collaboratively, while supportive psychotherapy builds the trust necessary for exploring difficult topics. Peer support from others with similar experiences provides powerful validation and hope.
Some individuals also find that medication, when used alongside these therapeutic approaches, can enhance their ability to engage with treatment and develop insight. Even without full awareness, many achieve meaningful recovery and improved functioning through consistent therapeutic engagement.
How should I respond when my loved one insists their delusions are real?
Avoid directly contradicting delusions, as this typically damages trust without changing beliefs. Instead, validate the emotional reality behind their experiences—the fear, confusion, or suspicion—while gently introducing alternative perspectives.
Use phrases like “I understand this feels completely real to you,” followed by “I wonder if there might be another explanation we could explore together.” Focus on the impact their experiences have on their life rather than debating whether the experiences are real.
Encourage engagement with therapeutic support where trained professionals can use evidence-based approaches like CBT for psychosis to help your loved one examine their beliefs in a safe, non-confrontational environment.
How can AMFM help someone with schizophrenia who lacks insight into their condition?
AMFM provides specialized residential treatment designed to support individuals with schizophrenia, including those with limited self-awareness. Our approach focuses on building trust and addressing expressed needs rather than demanding acceptance of illness.
We utilize evidence-based therapies proven effective for improving insight, including CBT for psychosis, supportive psychotherapy, peer support programming, and family therapy. With 24/7 care, daily life skills training, experiential therapies, and comprehensive psychosocial support, AMFM creates an environment where therapeutic progress can occur even before complete insight develops.
Our clinical team understands how to work compassionately with anosognosia, meeting individuals where they are and supporting gradual development of self-awareness through consistent, non-confrontational therapeutic engagement.













